Health Equity | The Social Determinants of Health | Our Commitment
OPGHI offers a wide range of mental and musculoskeletal health care services informed by best practices, designed to address the structural drivers of health equality. Using innovative care models to improve patient health outcomes we can simultaneously treat patients and train future health professionals on the multidisciplinary care necessary to end health disparity. In doing so we enrich patient and provider support through partnership, education, inclusion, and advocacy.
What is Health Equity?
According to the World Health Organization, Health Equity is defined as “the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically or by other means of stratification. ‘Health equity’ or ‘equity in health’ implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential.” 1 “Equity in health implies that ideally everyone should have a fair opportunity to attain their full health potential and, more pragmatically, that none should be disadvantaged from achieving this potential.” 2 Health Equity is driven by a number of things.

Figure 1 – Social Determinants of Health
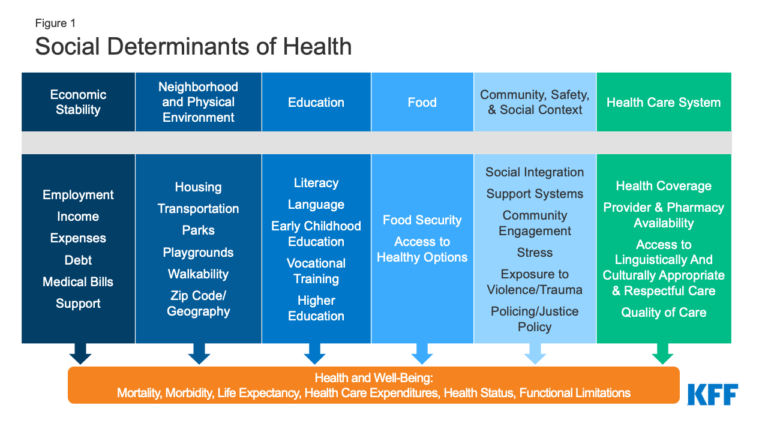
Figure 2 – Social Determinants of Health
Social Determinants are the circumstances or situations having significant impact on a person’s overall health and wellbeing. The conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. 3 The U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion has classified these into 5 categories:
1. Economic Stability (examples include)
- a. Employment
- b. Income
- c. Expense
- d. Debt
- e. Medical Bills
- f. Support
2. Education Access and Quality (examples include)
- a. Literacy
- b. Language
- c. Early Childhood Education
- d. Vocational Training
- e. Higher Education
3. Healthcare Access and Quality
- a. Healthcare Coverage
- b. Provider & Pharmacy Availability
- c. Access to linguistically and culturally appropriate and respectful care
- d. Quality of Care
4. Neighborhood and Built Environment (examples include)
- a. Housing
- b. Transportations
- c. Parks
- d. Playgrounds
- e. Walkability
5. Social and Community Context
- a. Social Integration
- b. Support Systems
- c. Community Engagement
- d. Stress
- e. Exposure to Violence
- f. Policing/Justice Policy
The Kaiser Family Foundation takes this one step further to include an additional
category known as Food Security.
6. Food
- Food Security
- b. Access to healthy options
1 https://www.who.int/health-topics/health-equity#tab=tab_1
2 Whitehead M. The concepts and principles of equity and health. Int J Health Services. 1992;22:429–445
3 Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Retrieved [date
graphic was accessed], from https://health.gov/healthypeople/objectives-and-data/social-determinants-health
-
Our Commitment to Addressing
Social Determinants of Health
OnePatient Global Health Initiative recognizes simultaneous societal oppression and privilege as it relates to the provision of healthcare. We are committed to the importance of our roles by acknowledging and addressing our own belief systems and how they impact patient wellness. We strive to understand how healthcare systems work, as well as our place in those systems, and commit to evaluate and improve on any societal disadvantage impacting patient health


Core Area 1: Economic Stability
- Increasing employment potential in those with physical and mental health concerns by improving access to and provision of mental and specialty health services in underserved communities.
- Reducing the number of patients with arthritis, who are unable to work or work without limits.
- Working to reduce work related injuries that result in missed work.
Core Area 2: Healthcare Access
- Providing access to specialty musculoskeletal and behavioral health care in underserved communities.
- Working to improve patient understanding of health concerns, compliance with, potential treatments and collaborative plans of care, to involved outcomes.
- Providing access to specialty substance use care in underserved communities.
- Established comprehensive preventative programs to address opioid screening, with ongoing monitoring.
- Improved health care prevention through education and monitoring
- Opened lines of communications where patients collaborate with providers.
- Verifying patient understanding and compliance at every visit.
Core Area 3: Education Access and Quality
- Providing access to high quality training programs for medical and counseling students.
- Biopsychosocial interdisciplinary treatment model addressing full scale patient needs.
- Training future clinicians on the importance of a multidisciplinary approach to health.
- Educating and encouraging patient use of multidisciplinary resources in medicine.
Core Area 4: Neighborhood/Community Programs
- Created community partnerships for areas of resource.
- Started telehealth smoking cessation groups
- Started telehealth group for behavioral management of weight.
- Started telehealth support groups for grief, loss. and pain.
Core Area 5: Social and Community Context
- Provided screenings for depression, anxiety and substance use.
- Increased patient health literacy within the patient resource portal.
- Providing advocacy services for all psychosocial and medical concerns.
- Conducting preventative screening for opioid dependency.
- Referrals for other medical concerns.
Core Area 6: Food Security
- Provide access to behavioral health supports for weight loss and management.
- Provide resources for meal preparation including cooking tutorials.
- Provide workshops on understanding nutritional labels.
Schedule Your Consultation
Book your appointment with our skilled medical team, whether in person or over the phone, and set off on the path to a healthier future.


