The connection between childhood trauma and ADHD (Attention Deficit Hyperactivity Disorder) has become an increasingly important topic in mental health discussions. Navigating adulthood with the symptoms of ADHD or the lingering effects of childhood trauma can be an overwhelming experience. What makes it even more challenging is that the two often share many similarities in how they affect behavior, emotional regulation, and day-to-day functioning. For adults who have struggled with focus, emotional swings, and impulsivity, the question often arises: Is this ADHD, trauma, or both?
Understanding the overlap between childhood trauma and ADHD, especially later in adulthood, is essential for developing effective coping strategies. While getting the right diagnosis matters, there’s also immense value in focusing on symptom management rather than becoming overly concerned with whether ADHD or trauma is the primary cause.
How ADHD and Childhood Trauma Overlap
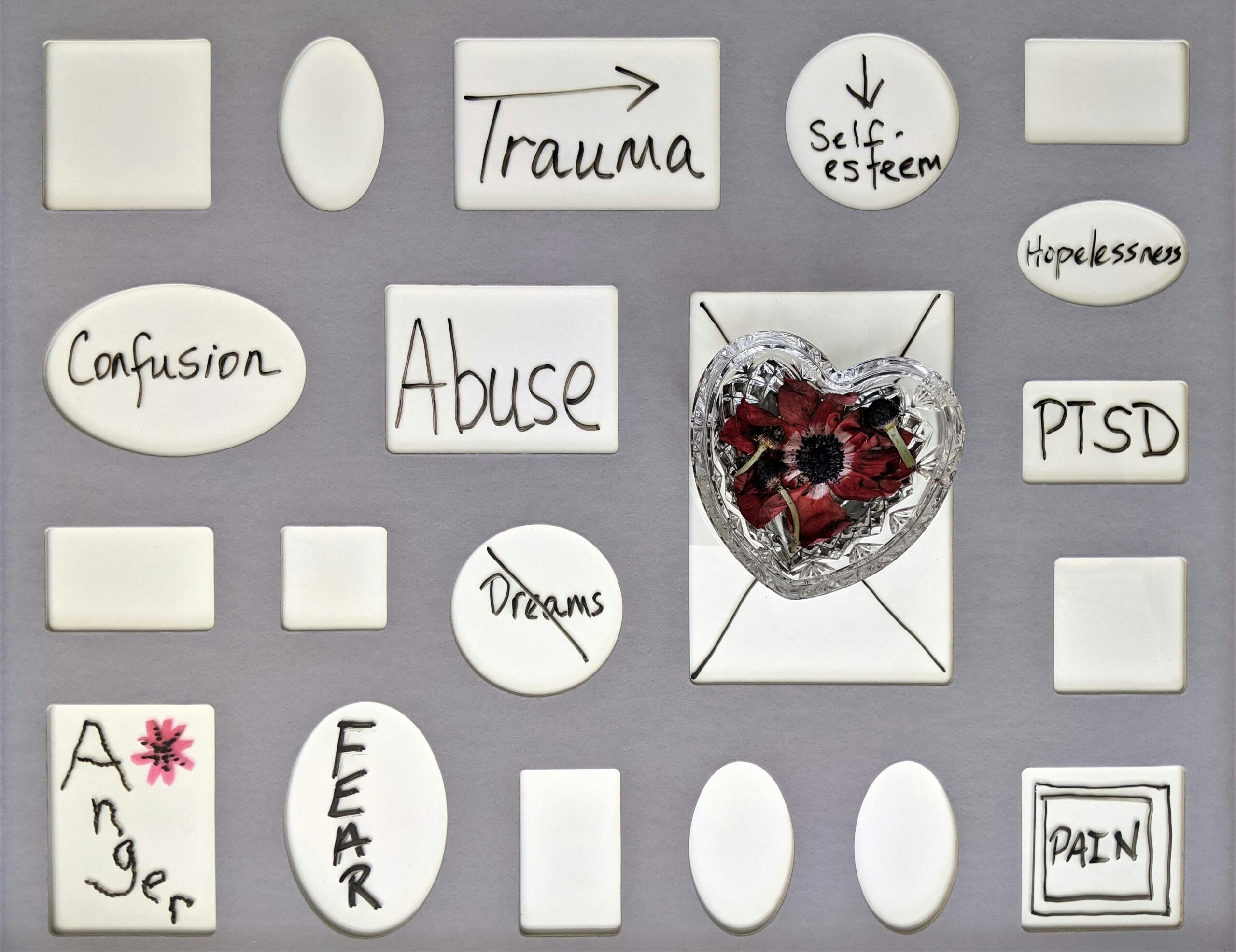
To start, it’s important to recognize that both ADHD and childhood trauma affect the brain, albeit in different ways. ADHD is typically seen as a neurodevelopmental disorder, usually diagnosed in childhood, that affects attention, impulse control, and executive function. Childhood trauma, on the other hand, impacts emotional and psychological development and can lead to long-term effects such as anxiety, hypervigilance, and emotional dysregulation. Trauma is often categorized under PTSD (Post-Traumatic Stress Disorder) or complex PTSD, especially when it stems from repeated or prolonged experiences.
Both ADHD and trauma can lead to behaviors that overlap significantly:
- Inattention and distractibility: Adults with ADHD frequently find it hard to focus on tasks or stay organized. Similarly, trauma survivors may struggle with focus, often due to their minds being preoccupied with anxiety, intrusive memories, or heightened stress responses.
- Emotional dysregulation: Mood swings, irritability, or emotional outbursts are common in both ADHD and those who have experienced trauma. An adult with ADHD may struggle with emotional control due to executive functioning deficits, while someone with trauma may be responding to triggers or unresolved emotional pain.
- Impulsivity: Impulsive decisions, acting without thinking, or struggling to maintain long-term commitments can be signs of ADHD. However, for trauma survivors, these behaviors may be tied to coping mechanisms developed in response to feelings of powerlessness or the need to regain control over their lives.
- Hyperactivity or restlessness: While hyperactivity is a hallmark of ADHD, trauma survivors often exhibit similar symptoms, particularly in the form of nervous energy, fidgeting, or feeling constantly on edge due to lingering hypervigilance or anxiety.
- Memory and executive function issues: ADHD is known to impair working memory and organizational skills, making it hard for adults to stay on top of everyday tasks. Trauma can also affect memory, particularly when the brain is in survival mode, leading to forgetfulness or difficulty concentrating.
These similarities make it difficult to differentiate between ADHD and trauma, especially when they’ve both been part of someone’s life for a long time.
Which Came First: ADHD or Trauma?
The question of which came first—ADHD or childhood trauma—is not easy to answer, and in some cases, it may not be necessary to pinpoint the exact origin. Both conditions can coexist and even exacerbate one another.
- ADHD making someone vulnerable to trauma: Adults who have ADHD, particularly those diagnosed later in life, may have experienced difficulties in school, social situations, or relationships due to their symptoms. These struggles could make them more vulnerable to traumatic experiences like bullying, emotional neglect, or unstable relationships.
- Trauma mimicking ADHD: On the other hand, a child who experiences trauma might display symptoms that look like ADHD. For example, a child who is constantly anxious or in a state of hypervigilance may seem inattentive or restless, much like a child with ADHD. Over time, these symptoms can become ingrained and persist into adulthood, even if the trauma occurred years earlier.
The fact that trauma affects brain development, especially in early childhood, complicates the picture even further. Repeated exposure to stress can change how the brain processes emotions and manages attention, making it look very similar to ADHD in later life.
Diagnosing ADHD or Trauma in Adulthood
For adults seeking answers to their long-standing difficulties with focus, impulse control, or emotional regulation, the path to diagnosis is often unclear. Clinicians face a challenge in distinguishing between ADHD and trauma because the two conditions not only overlap but may coexist.
Adults with undiagnosed ADHD may go years believing their difficulties stem solely from traumatic experiences, and vice versa. The challenge for clinicians is to dig deep into personal history, examining not just current symptoms but the context in which they developed.
Key questions a professional might ask include:
- When did the symptoms first appear? Did they start in childhood, or did they develop after a particular traumatic event?
- Are the symptoms consistent across different environments, or do they flare up in certain situations?
- How do current life stressors or triggers impact the symptoms?
Given how intertwined ADHD and trauma can be, some people may receive a dual diagnosis, which acknowledges the influence of both.
Managing Symptoms Without Getting Hung Up on the Diagnosis
While understanding whether your symptoms are due to ADHD or trauma can be helpful, it’s important not to get stuck on the label. Focusing too much on which diagnosis applies can sometimes divert attention away from what really matters: managing symptoms and improving quality of life. Here are some practical strategies for adults dealing with these overlapping challenges:
- Emphasize Structure and Routine
Both ADHD and trauma can cause problems with organization and focus. Creating a structured daily routine can help provide the predictability that the brain craves. Use tools like planners, reminders, and apps to stay on track with tasks, and break larger tasks into smaller, manageable steps.
- Work on Emotional Regulation
Emotional outbursts, impulsivity, and difficulty managing stress are common for both conditions. Mindfulness techniques can help you calm your mind and become aware of emotional triggers without reacting impulsively and starting an emotional spiral. Use deep breathing or grounding techniques to calm yourself in stressful moments. One example is the 5-4-3-2-1 grounding technique to reconnect you with the present through your 5 senses, where you identify:
- 5 things you can see
- 4 things you can feel
- 3 things you can hear
- 2 things you can smell
- 1 thing you can taste
- Exercise Regularly
Physical activity can help regulate both ADHD and trauma symptoms by reducing stress, improving focus, and enhancing mood. Exercise releases endorphins, which can counteract feelings of anxiety or restlessness. Activities like yoga, running, or even regular walks can significantly benefit mental health.
- Identify and Avoid Triggers
For trauma survivors, specific environments or experiences may trigger symptoms of anxiety or hypervigilance. Identifying these triggers and learning ways to manage or avoid them can help reduce the impact of trauma-related symptoms. Similarly, those with ADHD may notice patterns of distraction or impulsivity in certain settings and can work to reduce these triggers.
- Seek Professional Support
If managing symptoms on your own becomes overwhelming, seeking professional support is always a smart choice. Whether through therapy, coaching, or medication, professionals can help develop a tailored plan for managing symptoms. Trauma-focused therapy, such as EMDR (Eye Movement Desensitization and Reprocessing), can help individuals process unresolved trauma, while medication like stimulants may be used to address ADHD symptoms.
Behavioral therapies, such as Cognitive Behavioral Therapy (CBT), can also be highly effective for both ADHD and trauma. CBT teaches individuals to identify unhelpful patterns of thinking and behavior and replace them with healthier alternatives. This can be particularly helpful for reducing impulsivity and emotional dysregulation.
- Practice Self-Compassion
Dealing with ADHD or trauma, or both, can be exhausting. It’s important to practice self-compassion and avoid negative self-talk. You need to feel safe and supported in order to heal. Do your best to create a nurturing, non-judgmental environment for yourself to reduce stress. This might include positively reinforcing yourself when you accomplish a task, setting clear but flexible goals or expectations for yourself, and offering yourself empathy. Understand that managing these conditions is an ongoing process, and setbacks are part of the journey.
Conclusion
Whether ADHD or childhood trauma is driving your symptoms in adulthood, focusing on practical, symptom-based management strategies is the most effective way to improve your well-being. The overlap between the two conditions makes it difficult to draw clear diagnostic lines, but the good news is that both ADHD and trauma respond well to similar interventions. By creating structure, practicing emotional regulation, and seeking professional support when needed, adults can learn to manage their symptoms and lead fulfilling lives—without becoming overly hung up on whether it’s ADHD, trauma, or both.
To schedule an appointment with OnePatient, contact info@onepatient.org.